A recent study in mice led by the University of Notre Dame found that a new antibiotic was more effective than first-line antibiotics for C. difficile infection and significantly reduced the risk of reinfection. The findings were published in the Proceedings of the National Academy of Sciences (PNAS).

Symptoms caused by C. difficile include abdominal cramps, diarrhea and fever, and in extreme cases can lead to severe dehydration and kidney failure. In the United States alone, 13,000 people die each year from these infections. As a result, the Centers for Disease Control and Prevention has listed it as one of the five antibiotic-resistant infections that are an "urgent threat”.
The study's corresponding author, Mayland Chang of the University of Notre Dame, noted that C. difficile infections cause more than seven times as many deaths as the other four infectious diseases that pose an urgent threat. C. difficile usually infects the intestines after people take antibiotics to clear another infection. When people inhale airborne spores in the hospital, C. difficile is allowed to take up residence as the antibiotics eliminate the gut microbiota. Clinically, the first-line antibiotic vancomycin works well for initial C. difficile infections, but is not as effective for follow-up.
Alexander Khoruts, University of Minnesota, said vancomycin is not active against spores, and recurrence of C. difficile infection remains a major problem after a course of vancomycin. This means that C. difficile spores can be silently present in the body and cause infection years later, Chang said, adding that about 25 percent of people infected with C. difficile will go on to become infected a second time, 40 percent of those infected a second time will have a third infection, and 65 percent of those infected a third time will have a fourth infection.
Chang's team tried to break the reinfection cycle. They searched a database of antimicrobial molecules for compounds active against a specific binding protein in C. difficile and came up with two compounds: oxadiazole 1 and oxadiazole 2. In in vitro tests, both compounds killed C. difficile when used at the same concentration as vancomycin. Oxadiazole is rapidly absorbed into the bloodstream, but this is problematic for intestinal infections, which require the drug to remain in the intestine. Oxadiazole 2 enters the bloodstream of mice quickly, so the team did not study it further. Oxadiazole 1, however, is not absorbed into the bloodstream. In a series of C. difficile infection studies, the researchers found that oxadiazole 1 protected mice from death 30% better than vancomycin.
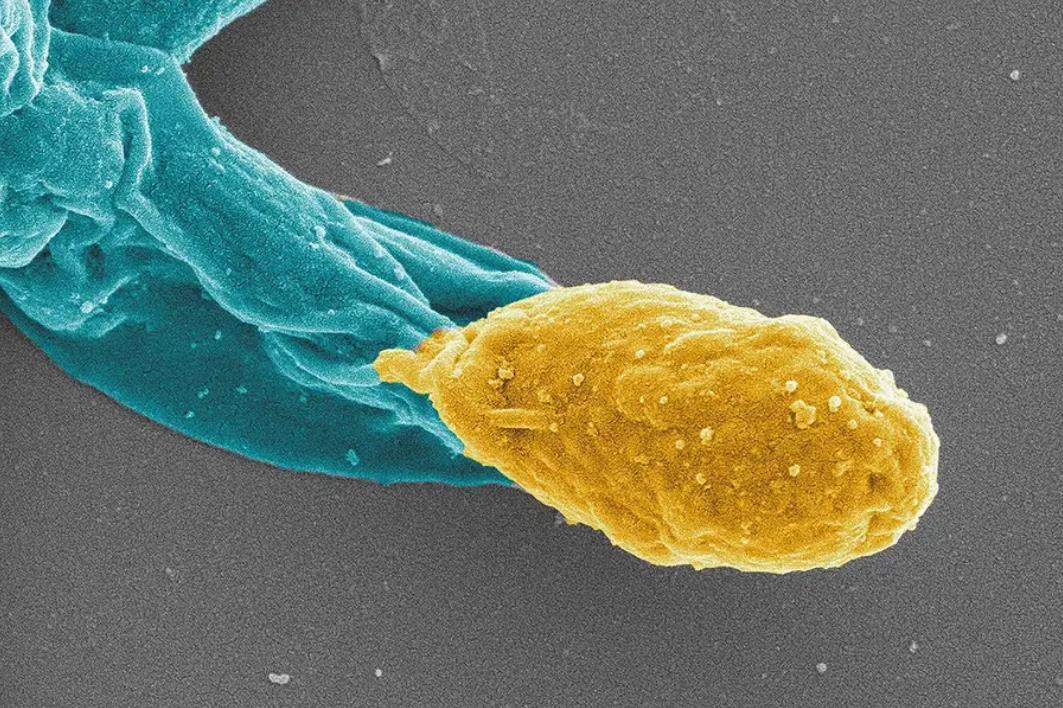
A new antibiotic effectively treats C. difficile infection in mice and helps prevent the formation of new spores (yellow part of the figure)
Perhaps the most promising outcome is the way in which the drug can stop persistent infections. Oxadiazole 1 blocks two proteins that help C. difficile form drug-resistant spores. Three weeks after treatment, mice treated with vancomycin still had detectable spores in their feces and continued to have recurrent infections. Mice treated with oxadiazole 1 had no quantifiable spores detected and no reinfection during the study period.
This finding may suggest a new approach to treating C. difficile infections in humans. Another promising treatment currently available is fecal microbiota transplantation, in which patients receive fecal microbes from uninfected donors to re-establish a healthy intestinal microbiota.
Recently, the U.S. Food and Drug Administration has approved two commercially available drugs based on fecal microbiota transplantation, but these drugs are not always effective. khoruts believes that new drugs need to be developed to treat C. difficile.
A dual-action antibiotic that kills Clostridioides difficile vegetative cells and inhibits spore germination
Journal: PNAS
Corresponding author: Mayland Chang
Abstract:
Clostridioides difficile infection (CDI) is the most lethal of the five CDC urgent public health treats, resulting in 12,800 annual deaths in the United States alone [Antibiotic Resistance Threats in the United States, 2019 (2019), www.cdc.gov/DrugResistance/Biggest-Threats.html]. The high recurrence rate and the inability of antibiotics to treat such infections mandate discovery of new therapeutics. A major challenge with CDI is the production of spores, leading to multiple recurrences of infection in 25% of patients [C. P. Kelly, J. T. LaMont, N. Engl. J. Med. 359, 1932–1940 (2008)], with potentially lethal consequence. Herein, we describe the discovery of an oxadiazole as a bactericidal anti-C. difficile agent that inhibits both cell-wall peptidoglycan biosynthesis and spore germination. We document that the oxadiazole binds to the lytic transglycosylase SleC and the pseudoprotease CspC for prevention of spore germination. SleC degrades the cortex peptidoglycan, a critical step in the initiation of spore germination. CspC senses germinants and cogerminants. Binding to SleC is with higher affinity than that to CspC. Prevention of spore germination breaks the nefarious cycles of CDI recurrence in the face of the antibiotic challenge, which is a primary cause of therapeutic failure. The oxadiazole exhibits efficacy in a mouse model of recurrent CDI and holds promise in clinical treatment of CDI.